Perinatal Mental Health: Questions and Answers About PMADs
PMADs (or perinatal mood and anxiety disorders) are mental health conditions that occur around having a child. The typical definition includes onset within one year. They can occur in birthing people, partners, adoptive parents, and people struggling with infertility.
There are a lot of misconceptions about PMADs, so let’s dive in to the most common questions we get about PMADs, some symptoms and risk factors, and where to go to get help:
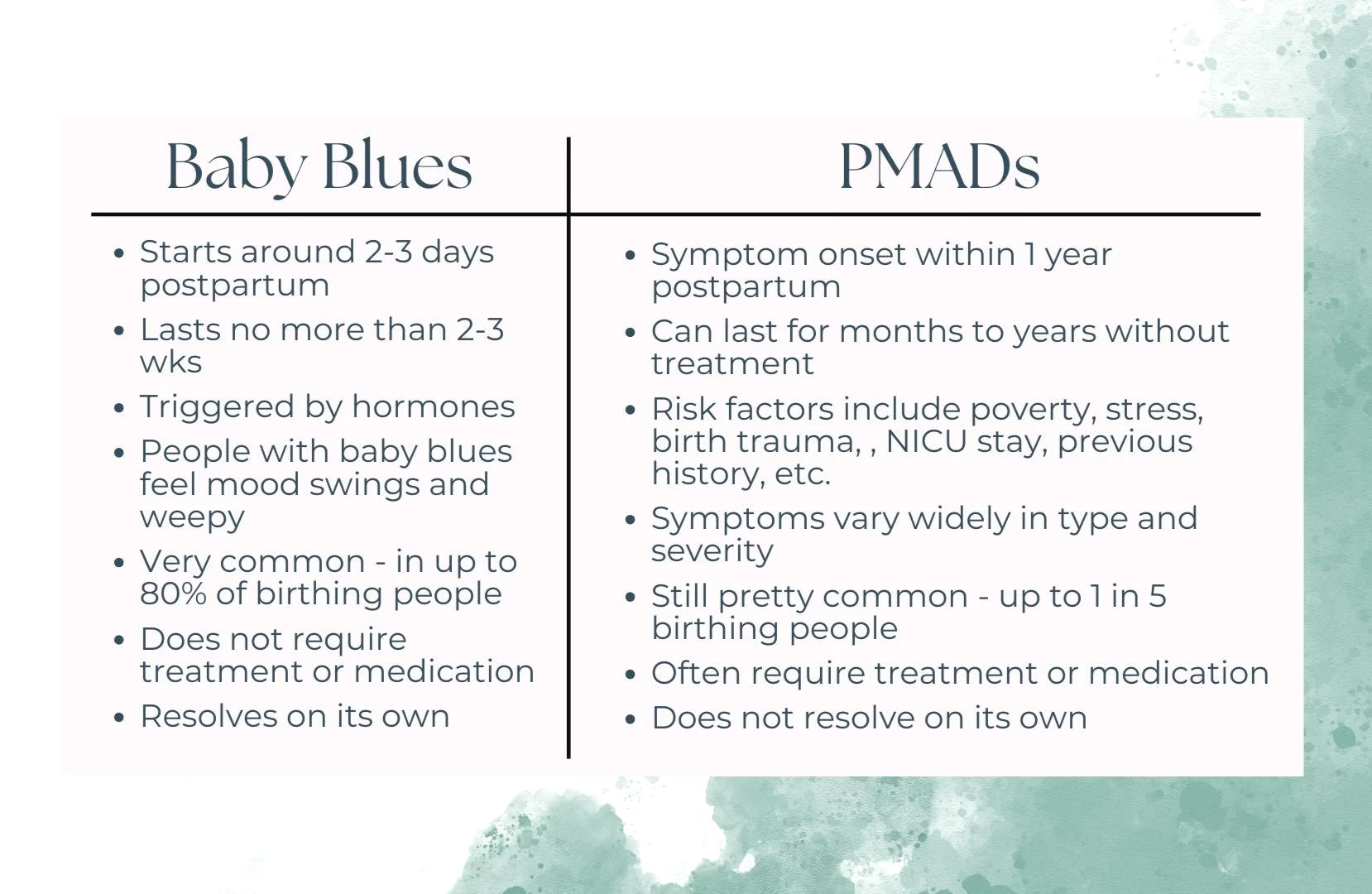
Are PMADs the same as the baby blues?
In short, nope.
PMADs can occur during pregnancy or postpartum, and include diagnoses like:
Yikes. Those all sound scary. It can feel overwhelming and scary. But that's why we're here - to sort through the scary things and help people get what they need to feel better.
Remember, You are not alone: Up to 1 in 5 birthing people and 1 in 10 partners meet criteria for a PMAD*
(*Honestly I suspect it's higher for everybody, but rates for LGBTQ+ and BIPOC parents are even higher. The existing research does not capture these disparities adequately.)
WHOA. If rates are that high, why aren't we talking more about it?
In 2019, less than 20% of postpartum people were screened for PMADs.
And less than 30% of people who screen positive for postpartum depression or anxiety actually receives treatment.
Why? Mental health stigma, systemic issues like racism, lack of screening, lack of trained providers, finances, and more impact awareness and access to services.
The takeaway of all of that is PMADs are quite common. You are not alone in struggling, even if it feels like everybody else is doing fine.
Note: a lot of people with PMADs look or act "fine". ASK your friends and family how they're really doing.
So how do you know if you have a PMAD?
Let’s take a look at some of the most common PMADs and how they might feel if you are experiencing it:
What are the risk factors for PMADs?
The words "risk factor" can sound scary, but we like to think of it as a heads up to pay a little extra attention. Remember: the more we know, the more we can make plans to cope, keep an eye on things, or get extra help when needed.
Some of the most common risk factors for postpartum depression, anxiety, & OCD include:
A personal or family history of depression, anxiety, OCD, or postpartum depression/anxiety
Premenstrual dysphoric disorder (PMDD or PMS)
Inadequate social or partner support
Financial or relationship stress
Complications in pregnancy, birth, or breastfeeding
A major recent life event: loss, house move, job loss, breakup
Parents of multiples or NICU parents
People who’ve gone through infertility treatments
Risk Factors for Post Traumatic Stress Disorder mostly center on HOW your birth went, and if it was traumatic, or if at any time you believed that you or someone else were in danger. The risk factors for Postpartum PTSD include:
Perceived stress or trauma, typically surrounding birth experience
Prolapsed cord or unplanned C-section
Use of vacuum extractor or forceps during delivery
Baby going to NICU
Feelings of powerlessness, poor communication and/or lack of support and reassurance during delivery
Previous trauma, such as rape or sexual abuse
Significant physical complications during pregnancy or childbirth
Risk Factors for Postpartum Psychosis
The most significant risk factors for postpartum psychosis are a personal or family history of bipolar disorder, or a previous psychotic episode.
Remember that Postpartum Psychosis is always a medical emergency and requires immediate medical evaluation.
There is unfortunately still often a lot of stigma associated with PPP, but very few people who suffer from PPP harm their children. Please know that if you have experienced PPP, it is not your fault and you are not a bad parent. We’re glad you’re still here.
Well that's all terrifying. Does having risk factors mean I'm for sure going to have a PMAD?
Nope. Some people have zero risk factors and have a PMAD, some have tons of risk factors and don't. But that's exactly why it's important to be informed - so IF it happens, you know how and where to get the help that you need. Because there IS help available, and you DESERVE to get the help you need.
I have some risk factors - so now what?
Talk to your support system. Have conversations early with your doctor/other providers, partner, family, or friends about the risk factors you have and what might indicate you need help. Consider making a postpartum plan for after birth that includes what steps might be helpful for you.
If you have had a previous PMAD, you can make a plan loosely based on your last experience, but know that your experience this time around may look completely different.
Some people also choose to start, restart, or tweak dosages of medication during pregnancy in preparation for after birth, or start meeting with a therapist if they are likely to experience a PMAD.
I think I have a PMAD. What do I do?
First, take a breath. You're still you even if you suspect you have a PMAD. This is just additional information. The purpose of learning this is so that you can get the help you need and feel better. What’s true is true regardless of a label.
You're not alone, PMADs don't make you a bad parent, and there is help available.
There are immediate resources available:
National Maternal Mental Health Hotline (24/7): 1-833-943-5746
PSI Warmline - 1-800-944-4773
MMHI (Milwaukee area, WI only)